There’s a Difference Between “Side Effects” and Signs You’re on the Wrong Medication
When you’re prescribed a new medication for depression, anxiety, or mood instability, you’re often told to expect some “side effects.” Maybe some nausea, some fatigue, or changes in appetite. You brace yourself. You wait it out. And maybe—hopefully—it helps.
But what if those “side effects” aren’t just annoyances to power through?
What if they’re your body’s way of saying:
This medication isn’t right for you?
What Does It Mean for a Psychiatric Medication to “Work”?
When people come to us at Colorado Mood Center, one of the most common questions we hear is:
“Will this medication work for me?”
It’s a fair—and important—question. But what does it actually mean for a psychiatric medication to “work”?
Many assume that “working” means the symptoms simply go away. But especially in complex mood conditions—like bipolar depression, agitated depression, or mixed states—the reality is often more nuanced.
Let’s break it down.
4-Dimensional Psychiatry: Why Medication Should Never Be on Autopilot
In psychiatry, time is not just a backdrop—it’s a treatment variable. Yet much of modern mental health care treats medications as if they exist in a vacuum: find the “right” one, set the dose, and let it run indefinitely. This static view doesn't match the complex and shifting reality of mental health. We call our approach 4-dimensional psychiatry because we believe that treatment should evolve with the patient over time—not in spite of change, but because of it.
Executive Dysfunction Is Not Always ADHD
Executive dysfunction is not always ADHD. In fact, it’s most likely not ADHD.
“Are Antidepressants Really Antidepressants?” Why SSRIs Might Be More Like Emotional Tylenol
When most people hear the word antidepressant, they think of a pill that lifts sadness or fixes chemical imbalances in the brain. And for some people, medications like Lexapro, Zoloft, or Prozac can help. But here’s a truth that may surprise you:
Serotonin-based antidepressants (SSRIs) aren’t really antidepressants. At best, they’re like emotional Tylenol.
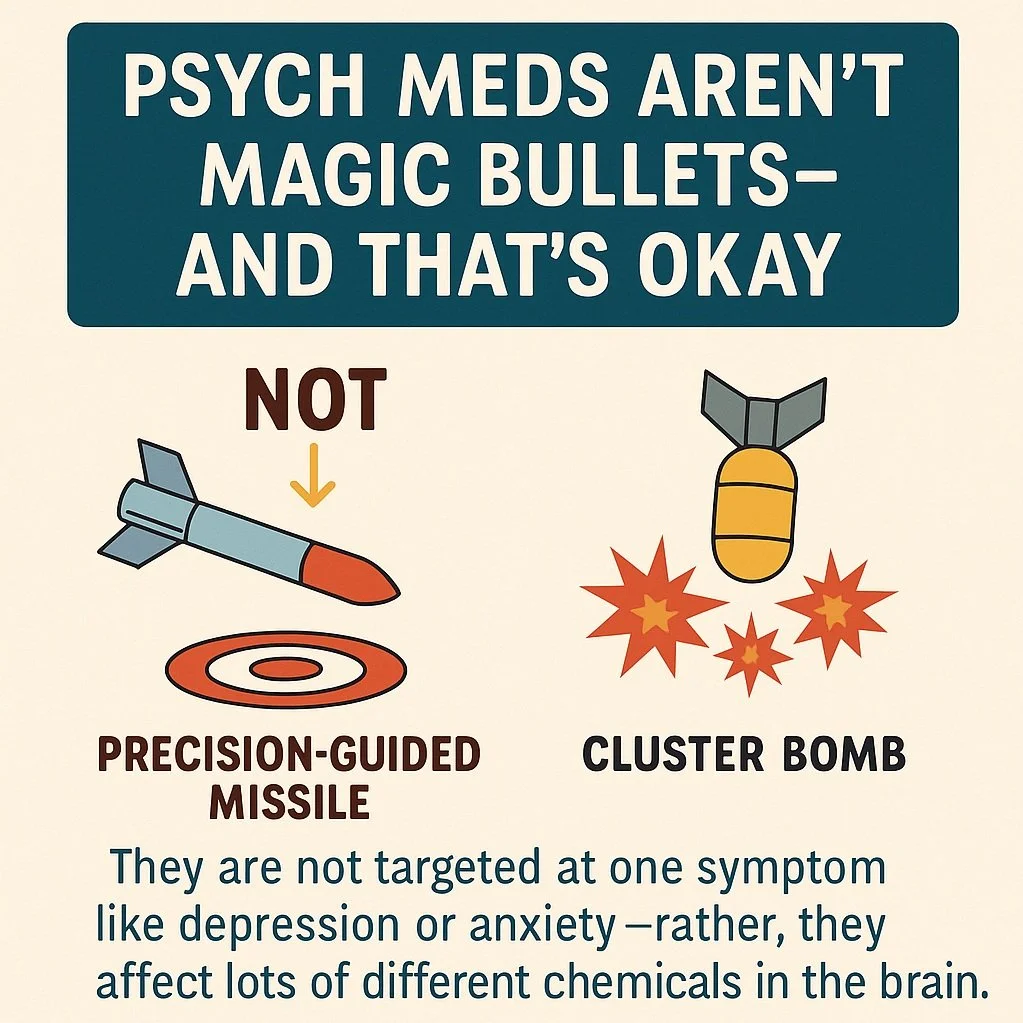
Psychiatric medications are not magic bullets - and that’s okay
When most people think about psychiatric medications, they imagine a simple fix: “I’m anxious, so I need an anti-anxiety medication,” or “I’m depressed, so I need an antidepressant.” It’s an easy story to believe—because that’s exactly how these medications are marketed. But the truth is more complicated. And honestly, more interesting.
When anxiety isn’t just anxiety: could it be a mixed state?
Most people recognize anxiety when they feel it: racing thoughts, a pounding heart, constant worry. It can feel overwhelming. But for some people, anxiety isn’t the whole story. It’s just one piece of a much more complicated mood picture—especially if that anxiety comes with irritability, insomnia, mood swings, or sudden bursts of energy. In these cases, the anxiety may not be a standalone condition at all. It could be a sign of a mixed state.
How to tell if you’re on the wrong anti-depressant
Antidepressants can be life-changing. But they can also feel like a bad match—sometimes in ways that are subtle, confusing, or easy to brush off.
If you’ve been prescribed an antidepressant and something doesn’t feel right, trust that instinct. There’s a difference between side effects you can manage and a medication mismatch that’s quietly making things worse.